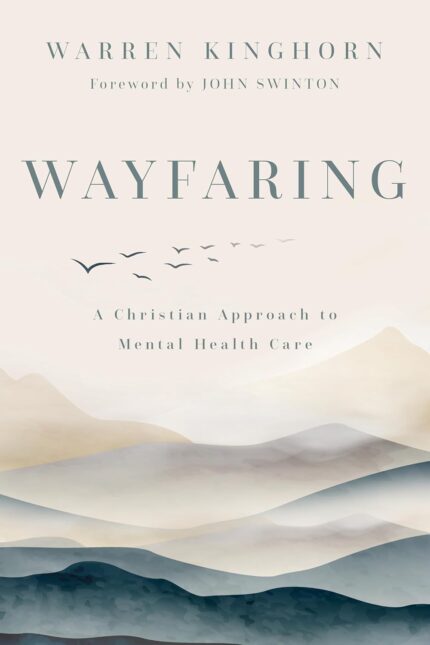
A theologically and scientifically engaged exploration of modern mental health care
The current model of mental health care doesn’t see people: it sees sets of symptoms that need fixing. While modern psychiatry has improved many patients’ quality of life, it falls short in addressing their relational and spiritual needs.
As a theologian and practicing psychiatrist, Warren Kinghorn shares a Christian vision of accompanying those facing mental health challenges. Kinghorn reviews the successes and limitations of modern mental health care before offering an alternative paradigm of healing. Based in the theology of Thomas Aquinas, this model of personhood affirms four truths: We are known and loved by God. We are creatures made of earth who are formed in community. We are wayfarers on a journey. We are called not to control, but to wonder, love, praise, and rest.
Drawing on theological wisdom and scientific evidence, Kinghorn reframes our understanding of mental health care from fixing machines to attending fellow wayfarers on the way to the Lord’s feast. With gentle guidance and practical suggestions, Wayfaring is an essential resource for pastors and practitioners as well as for Christians who seek mental health care.
From the Publisher


What People are Saying






Excerpt from chapter 1, “Modern Mental Health Care and the Machine Metaphor”
It is eight o’clock on a Thursday morning, and as usual, I am about to begin seeing outpatients in the Mental Health Clinic at the Durham VA Medical Center, where I serve as a staff psychiatrist. The examination room, located below ground level, is windowless, but I have done my best to humanize it, adding bookshelves and some framed artwork to supplement the plexiglass enclosed impressionist prints that the hospital installed long ago. I sit in an office chair with a monitor containing the electronic medical record close at hand, looking at the small sofa and chair that my patients, and sometimes their families, will occupy. Then I begin.
During the morning, I see seven to eight patients in thirty-minute slots—a luxury of time in an era where psychiatrists often spend ten to fifteen minutes with many of their patients for brief med checks. But the stories always exceed whatever time is allotted. Over the course of the morning I hear many stories, stories of pain, frustration, and sometimes of delight and triumph. I hear stories of grief and loss, of battle buddies who never returned from war, of children who died too soon from drug overdoses and motor vehicle accidents. I hear stories of sexual assault and intimate partner violence, sometimes told in detail. I hear stories of parents who drank too much and of childhood neighborhoods from which the rigors of military basic training were a welcome and dignifying relief. I hear stories of chronic pain, chronic loneliness, and hopelessness in the face of mounting chronic medical conditions. I hear stories of feeling anxious or depressed for no apparent reason at all. I hear stories of financial stress and reliance on disability income that requires the ongoing presence of symptoms. I hear stories of marriages and other intimate relationships: close and supportive relationships, loveless and hostile relationships in which a couple share a house but not a life, volatile relationships full of passion and anger. And I hear excited and hopeful stories: of relationships healed, of housing secured, of sobriety maintained, of community found, of spouses and children and grandchildren cherished.
With each of my patients, I listen as closely as I can to these stories, and we talk about them. Then, around the fifteen-minute mark of our thirty-minute visit, I turn to a mental checklist of things that I’m expected to document by the end of the appointment. I ask about thoughts of suicide, about substance use, about sleep and mood, about violence at home. Turning to the electronic medical record, I review the patient’s electronic medication list, sometimes short and sometimes quite long, and ensure in a process called “medication reconciliation” that the list is accurate. I comply with clinical reminders and complete structured scales measuring symptoms and behavior. As required for coding and billing purposes, I assign a formal psychiatric diagnosis. More often than not, I discuss and prescribe medicines. All the time, I discuss other approaches to treatment, ranging from individual psychotherapy to group therapy to twelve-step groups to personal habits and practices. I make referrals when appropriate. I explore possibilities for expanding community ties and for cultivating meaningful and purposeful activity. I set a time for the patient to return, usually weeks or months in the future. Then I say goodbye and welcome my next patient.
I always feel tired at the end of a clinic session. The stories overwhelm. I cannot contain them, no matter how hard I try. I reflect on the deep privilege of being entrusted with those stories. I marvel that people trust me to walk alongside them, trust me with some of the deepest and most hidden shadows of their lives. But the stories are so complex, their pain and struggle so pervasive, that I cannot help but wonder, What am I doing? What is it for? And is it for the good?


Author Bio
Warren Kinghorn is a psychiatrist and theological ethicist whose work centers on the role of religious communities in caring for persons with mental health problems and on how Christians engage practices of modern health care. Jointly appointed to the faculties of Duke Divinity School and the Department of Psychiatry and Behavioral Sciences of Duke University Medical Center, he is codirector of the Theology, Medicine, and Culture Initiative at Duke Divinity School and practices psychiatry at the Durham VA Medical Center.
Publisher : Eerdmans (July 11, 2024)
Language : English
Paperback : 312 pages
ISBN-10 : 0802882242
ISBN-13 : 978-0802882240
Item Weight : 9.6 ounces
Dimensions : 6.03 x 0.73 x 8.97 inches